Towards A New Beginning
What is kidney (renal) failure/injury?
Kidney Injury/Failure can be acute, which means that the kidneys have suddenly stopped working. Acute Kidney Failure is potentially reversible.
Chronic Kidney Failure is a slow progressive and irreversible loss of kidney function.
What is chronic kidney disease (CKD) and what are the common causes of CKD?
Chronic kidney disease is the presence of functional or structural abnormality in the kidney for three months or longer. eg. presence of screening “Maker” such as protein in urine or having a decreased kidney function for more than 3 months.
There are many causes of CKD. The kidneys are most commonly affected by diseases, such as diabetes and high blood pressure.
Some kidney conditions are inherited (run in families). Others are congenital, i.e., individuals may be born with an abnormality that can affect their kidneys.
What is end stage kidney disease (ESKD)?
ESKD is a stage at which practically the entire kidney function is lost. On ultrasound examination, the kidneys are usually small and shrunken. The kidneys can be considered to be dead for all practical purposes. Life long dialysis or transplantation becomes mandatory for survival. Each year approximately 350,000 – 400,000 people develop ESKD.
What are the signs and symptoms of kidney disease?
Kidney disease usually affects both kidneys. If the kidneys’ ability to filter the blood is seriously compromised by the disease, then wastes and excess fluid may build up in the body. Although many forms of kidney disease do not produce symptoms until late in the course of the disease, there are six warning signs of kidney disease:
- Puffiness around eyes, swelling of hands and feet
- More frequent urination, particularly at night. Difficult or painful urination.
- Blood and/or protein in the urine
- High blood pressure
- A Creatinine & Blood Urea Nitrogen (BUN) blood test, above the normal range (BUN & creatinine are waste products that build up in the blood when the kidney function is reduced.)
What are the treatment options for ESKD?
There are only two options for End Stage Kidney Disease:
- Life Long Dialysis
- Kidney Transplantation
What is dialysis?
It is a process that removes the waste products and helps maintain the volume and composition of body water – the most important and indispensable function of the kidneys It does not help in blood formation and activation of vitamin D as is the case with normal kidneys. Hence supplementary therapy is required It does not improve the function of diseased kidneys
What are the types of dialysis?
There are two types of dialysis:
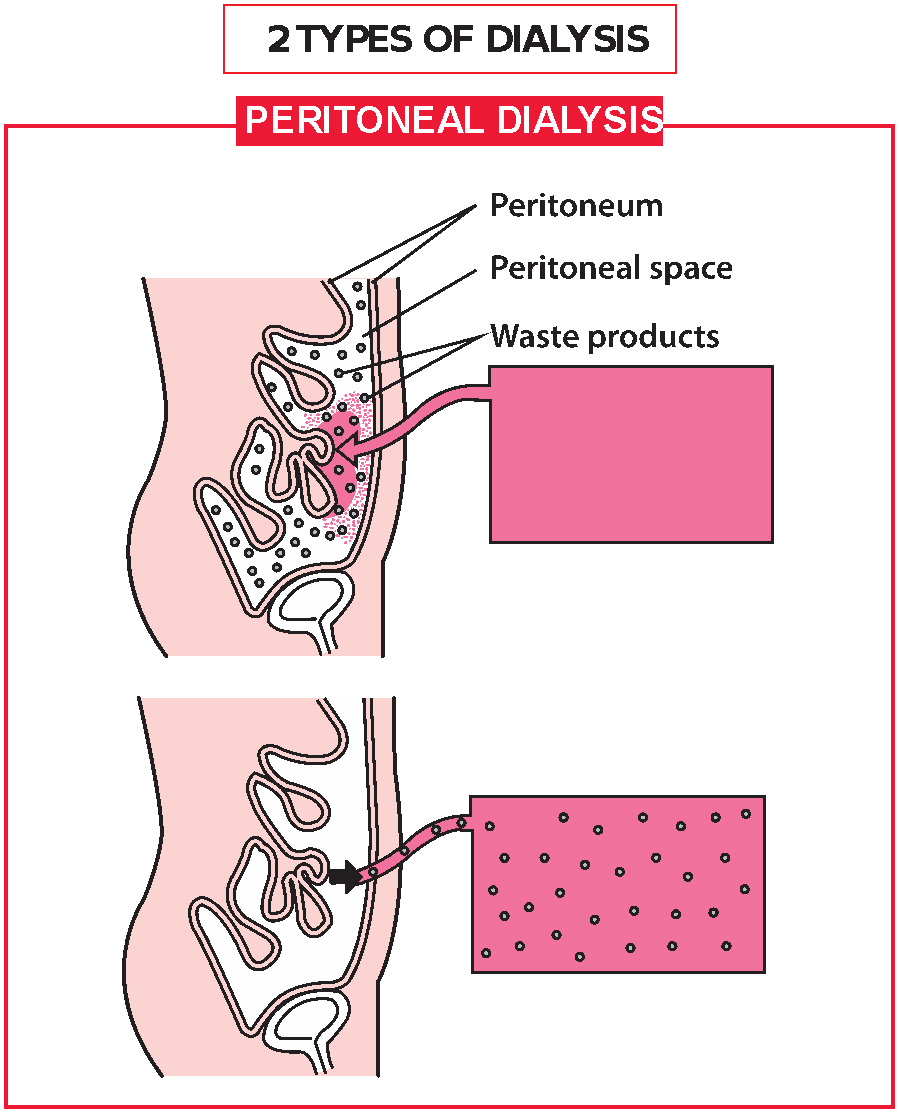
Haemodialysis, where the blood is cleaned outside the body via a machine Peritoneal dialysis, where the cleaning is done inside the body by the peritoneal membrane Occasionally, there may be medical reasons to prefer one dialysis over the other.
What is the best option for the treatment of ESKD?
Kidney (Renal) Transplantation is the best available treatment for ESKD because of the following reasons:
- Improved survival
- Better quality life
- Improved cost effective
Who is eligible for transplantation?
- All patients with ESKD should be assessed for suitability of kidney transplantation
- Patients having cancer or other active infections cannot go for transplantation
Special assessment is required for the following groups of patients:
- Old age
- Severe heart disease, lung disease or liver disease
- HIV positive patients
- Psychiatric Illness
Who can donate/give kidneys?
Living Donors
Indian Law permits near and dear ones to donate organs (kidney, liver, bone marrow). Parents, siblings, son, daughter, grandparents and spouse are treated as ‘near relatives’.
If a family member cannot donate a kidney because of difference in blood group and if there is another pair with a similar problem, the donors can be exchanged for the purpose of kidney transplantation. This is called a Swap Transplant.
Living donors are thoroughly investigated by the physician. The donors should be in good overall physical and mental health and free from uncontrolled high blood pressure, diabetes, cancer, HIV, hepatitis, and organ diseases (such as those related to the kidney, heart, liver, lung, intestine and pancreas). Living donors should be older than 18 years of age and compatible with the intended transplant candidate. The donors are screened from medical and psychosocial aspects.
Deceased Donor (Cadaver Donor)
A deceased donor is a person who is brain dead.
A person is dead when his heart stops beating permanently.
A person is dead even when the brain is dead but the heart is functioning. At this stage the heart can function for hours or days. During this period, if the family consents, various organs and tissues can be used for transplantation.
One can register for a cadaver organ with the ZTCC – Zonal Transplant Coordination Committee (city waiting list) through the Transplant Coordinator & the Nephrologist at the hospital.
What is the success rate of kidney transplantation?
- Overall, transplant success rates are very good
- Transplants from deceased donors have an 85 to 90% success rate for the first year. That means that after one year, 85 to 90 out of 100 transplanted kidneys are still functioning
- Live donor transplants have a 90 to 95% success rate. Long term success is good for people of all ages
What if my donor’s blood group does not match mine?
There are three options available for such patients:
- Blood group Incompatible transplantation ( ABOi)
- Living Donor Paired kidney exchange ( LDPE)
- Deceased donor ( cadaver) donor listing
What can my kidney donor expect?
The procedure for the person who is donating a kidney to you is exactly the same as for blood group compatible
donors. The special treatments are only necessary for you.
Is it expensive?
The cost of the kidney transplant surgery remains the same except that the cost of plasma exchange procedure is additionally to be calculated based on the amount of antibodies in your body.
Why Kokilaben Hospital?
The Nephrology and Urology departments boast of one of the largest dialysis units in the city and a sizeable renal transplant program, having performed both living and cadaveric transplants.
The stringent infection control practices, immunosuppressive protocols and proactive vigil for complications and their prompt management make the service comparable to the best. The Transplant Unit also integrates, analyses and addresses the health needs of the transplant patient and his or her family.
State-of-the-art procedures for kidney transplantation include:
- Cadaver Donor Kidney Transplantation
- Living Donor Kidney Transplants
- Paired Kidney Exchanges
- ABO-Incompatible Transplantation
- Laparoscopic Donor Nephrectomy
The Kokilaben Hospital Kidney Transplantation Team comprises of specialists in transplantation medicine and surgery. The team comprises of 2 nephrologists, 2 transplant coordinator and 3 transplant surgeons.


