MBBS, DCh, FCPS, DNB (Pediatrics)
Neonatal, Paediatric Critical Care and Paediatric Cardiac Critical Care
Specialised Services in Intensive Care Neonatal, Paediatric and Cardiac, Management and Treatment of Very Preterm Babies (completed 6 months of pregnancy or less than 1000 gm), Special types of Ventilation like High Frequency Ventilation & use of Nitric Oxide, Postoperative Cardiac Critical Care, Post operative Organ Transplant care ( Liver, Kidney, Lung and Heart), Ventricular Assist Device, Peritoneal and Haemodialysis including Hemofiltration, Extracorporeal Membrane Oxygenation (ECMO) –in Cardiac or Respiratory Failure
Fellowships: 2001-2007
Neonatal Fellowship:
Pediatric Intensive Care Fellowship
Pediatric Cardiac Critical Care Fellowship
Certificate Training:
Dr Preetha has pursued Post graduation degree in Paediatrics from Lokmanya Tilak Municipal Medical College-Sion. She also has experience of training and working in Australia and Canada for 7 years. She was the Chief Fellow in the Department of Paediatric Critical Care at Hospital for Sick Children, Toronto.
At KDAH, she manages Neonatal and Paediatric ICU which has Transport facility of Critically Ill Newborns and children up to 18 years. She was involved in the care of Preterm Quintuplets, 4 of the 5 babies survived and are thriving well at 7 years. She also looks after postoperative cardiac surgery patients in the Paediatric Cardiac ICU which sees 500 postoperative children per year.
This unit has looked after 2,400 sick newborns in the last 7 years with mortality rates less than 2.5 per cent
This unit has Managed 3,000 critically ill children in the last 7 years
She has been involved in the setting up of a state-of-the-art transport service for critically ill children. There is a dedicated neonatal and paediatric ambulance with neonatal transport incubators and neonatal and paediatric ventilators. Children are picked up from many peripheral hospitals and nursing homes in the outskirts of Mumbai.
Good baby care from Dr Preetha and Team with all the nursing staff of 9th floor pediatric zone.
Thank you for taking care of our baby and providing the necessary treatment. Special thanks to Dr Preetha J, Dr Sajeev V and their team.
I and Ajita, my wife, both want to thank you very sincerely for the life saving treatment given to our 33 weeks old pre mature born daughter. During her treatment at the hospital, we have witnessed the expertise, sincerity, openness, kindness o...
We just want to say a very special thanks to DR. PREETHA AND DR. VINAY JOSHI whom we will always be indebted to for saving the life of our child VIHAAN PRAMOD (diagonised with PPHN on birth) and giving him a new lease of life. When all hopes we...
Dear Mr. Narain,
I am writing to you to express my wife's and my gratitude for the wonderful care and attention provided to our darling daughter Avika during the 2 months she was in the NICU at your hospital.
...
| Conditions/Procedures | No. of cases treated | International success rate | KDAH success rate |
|---|---|---|---|
| Critically ill newborns | > 2400 | 97-98 per cent survival rate | 98.2 per cent survival rate |
| Severe Respiratory Failure managed with High Frequency Ventilation and inhaled Nitric Oxide | >50 | 60-70 per cent survival rate | 80 per cent survival rate |
| Acute Respiratory Distress Syndrome | >100 | 70-80 per cent survival | 80 per cent |
| Complex surgical problems | >300 | 80-90 per cent | 80 per cent |
| Congenital Diaphragmatic Hernia | >10 | 80 per cent | 90 per cent |
| Post Cardiac Surgery patients | >3000 | 80-90 per cent | 97 per cent |
Extracorporeal Membrane oxygenation (ECMO) is the only life-saving technology available to support and rest organs in case of organ failure- heart, lungs etc
Last month, we treated an infant 2 and a half month old- on ECMO-first of its kind in the country and the baby is going home.
We are at present treating a 9 yr old with ECMO and CRRT in a case of ARDS with multiorgan failure.
This has been achieved due to team effort by the entire PCICU, PICU team and especially Pediatric Cardiac surgeons, Perfusionists (who are working round the clock), the intensivists and the nursing team.
Mrs. Shreya Singh Jitan delivered a healthy baby boy (2.8 Kgs) today at 5.35 pm. She was with us in the hospital for 3 months (since Feb, 2011). She had presented with a pregnancy of six months (26 weeks - 600 gms) with a very short cervix and funnelling of internal os with bulging membranes (mouth of the womb was very short and open with the membranes bulging into it). This meant she would deliver very soon. At this stage one can put a stitch on the cervix called as a rescue cerclage of the internal os but due to the funnelling and bulging of membranes the water bag could easily burst, infection chances and a premature delivery are extremely high. Results with these cerclages are not very promising at such a stage. Maybe we could pull on for a few days only. The baby being extremely small (600gms) would have to spend many weeks in the ICU and dangers of prematurity like respiratory distress syndrome (breathing problems), hemorrhages (bleeding in the brain), feeding problems are possible and good outcome cannot be promised.
As against this we counselled her and her family, offered her a conservative management a stay in the hospital, antibiotics, head low position, uterine relaxants, Inj Betnesol inj (2) and vigilant care from the team which could carry on the pregnancy as far as possible.
We had done a similar plan for a patient Mrs ABC, last year and were successful. Since we are in a hospital with an excellent NICU team we were assured of the fact that we could do our best in case of a premature delivery. Our team of doctors headed by Dr Suchitra Pandit, Dr. Vinay & Dr. Preetha Joshi (baby doctors), Staff nurses, Radiologist Dr.Shefali Sardar, our junior doctors Jatinder, Deepali, Dimple were all very vigilant and offered reassurance at every visit. The family was told about the entire plan and they were very supportive.
We scanned her every fifteen days. The cervix got shorter & uterine pain was there but with medication we could avert labour.
It was only when we crossed 34 weeks ( 8 months) that we breathed a sigh of relief as lungs by then are mature. On 20th May, 2011 she was term and she was in early labour on 21st May. Short and sweet labour, a vacuum delivery - 2.8kgs baby boy.
What was very rewarding was the cooperation from the patient, the entire family. The family agreed and believe me as each week passed by we would pray that we sail through another week successfully.
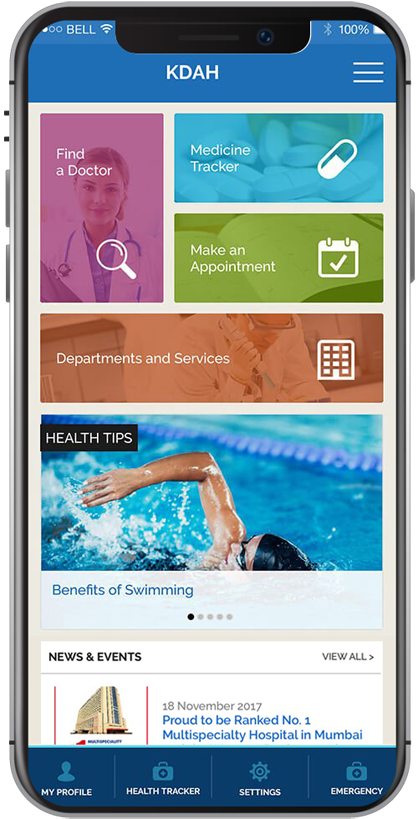
This appointment request is for regular consultation with the Doctor at Kokilaben Hospital, Four Bungalows. For online consultation, please CLICK HERE