
MS (Ortho), MRCS (UK), Fellow Spine & Scoliosis Surgery, USA
Spine surgery, Minimally invasive spine surgery, Scoliosis surgery
Minimally Invasive Spine and Scoliosis Surgery, Endoscopic spine surgery: Endoscopic decompression and diskectomy, Adult & Pediatric Spine surgery, Spinal trauma & tumor reconstruction, Cervical discectomy, Cervial Disc Replacement, Cervical Spine Foraminotomy, Cranio-Vertebral Junction (CVJ)pathologies, Minimal access spinal decompression Surgery (Laminectomy, Laminotomy), Minimal access Scoliosis correction (Scoliosis correction adult and pediatric), Minimal Lateral Access Spine Surgery, Minimally invasive Spinal Fusion ( TLIF), Advanced management of metastatic spinal tumors, Vertebroplasty and Kyphoplasty, Nerve Root Blocks Lumbar and cervical spine
Dr Abhijit Pawar has 15 years of experience in Orthopaedics and Advanced Spinal surgeries.
Dr Abhijit Pawar finished his Spine and Scoliosis surgery fellowship at the Hospital for Special Surgery (HSS) in, New York, United Stated from 2010-2012. HSS is well known Hospital for Orthopaedics and Spine Surgery in USA . He has worked with world renowned spine surgeons during his tenure.
Dr Abhijit Pawar got extensive training for 2 years in Spinal deformity and minimally invasive Spine Surgery. He was actively involved in more than 2000 Spinal Surgeries at HSS.
In 2009-2010 Dr Abhijit worked as a fellow in Spine surgery at University of Montreal Canada with Dr Hubert Labelle who heads the Spinal deformity study group in Canada.
In 2012-2013 he worked at the Albert Einstein School of Medicine in New York and Specialized in Paediatric Spinal Surgery. He actively performed more than 500 paediatric scoliosis surgeries. He also specialized in minimally invasive scoliosis correction.
He also worked with Dr Anthony Yeung in USA for some time and achieved expertise in endoscopic spinal surgery. Dr Abhijit Pawar specializes in stichless spine surgery under local anaesthesia for lumbar disc herniations.
After return from USA, he has performed more that 2000 Spinal surgeries in India.
His expertise is Minimally Invasive Spinal Surgery, Endoscopic spinal Surgery, Spinal deformity surgery and 3D Navigation guided Spine Surgery.
Dr. Abhijit Pawar guidance is just like family member, he is very confidant in his surgical new technology minimum invasive procedure
I recently had the privilege of being treated by Dr. Abhijit Y Pawar who is also a pioneer of 3d Navigation guided (O-Arm) spine and scoliosis surgery in India , I cannot express enough how grateful I am for the exceptional care I receive...
I recently visited Kokilaben Hospital for a spine surgery, and my experience was exceptional from start to finish. The check-in process was not so smooth as I was not advised on certain dos and don'ts.
The doctors and nurses were...
The overall procedure went smoothly. My mother was taken utmost care of. Dr. Abhijeet Pawar has been an excellent doctor in assisting my mother and has given clear insight throughout.
I, Mr. NIRIKO REBALY, Father of D’ANJARASOA NOMENJANAHARY Gicia Rebaly, de Madagascar, give all my gratitude and my regards to this hospital (KDAH), especially to all the doctors , who has given life to my daughter , and improved the heal...
A serious medical emergency is one which sends shivers thru the spine, literally a broken one. When my wife had a bad fall and after basic investigations when we consulted Dr Abhijit Pawar, the enormity of the problem she faced dawned upon us. ...
Hi,
Wanted to share my experience with Dr. Abhijeet Pawar. My father, Dr. Mohmad Sayed was suffering from severe pain in the left arm for over 4 months due to which he couldn't sleep for more than a couple of hours a day. So we consu...
| Conditions/Procedures | No. of cases treated | International success rate | KDAH success rate |
|---|---|---|---|
| Endoscopic spine surgery | 412 | 94-96% | 94% |
Spinal trauma |
329 | 80-85% | 82% |
| Minimal access spinal decompression Surgery | 300 | 98% | 98% |
| Minimally invasive Spinal Fusion ( TLIF). | 390 | 90-94% | 95% |
Vertebroplasty and Kyphoplasty. |
267 | 98% | 97% |
| Scoliosis correction adult and pediatric | 106 | 90% | 98% |
| Advanced management of metastatic spinal tumors | 138 | 70% | 80% |
| Cervical discectomy | 170 | 97% | 100% |
| Cervical posterior Minimal access decompressiom | 90 | 94% | 98% |
Cervial Disc Replacement |
12 | 92% | 100% |
| Nerve Root Blocks Lumbar and cervical spine. | 346 | 70% | 78% |
| Tumors and Infections | 140 | 80% | 90% |
13 year old girl presented to KDAH with history of Spinal deformity. She came with complaints of worsening for spinal deformity, rib hump and breast asymmetry. Scoliosis is a medical condition in which a person's spine has a sideways curve. The curve is usually "S"- or "C"-shaped. Scanogram X-ray of the Spine was done which showed severe spinal deformity with the main curve of thoracic spine measuring about 85 degrees. The proximal thoracic curve and the lumbar curve where also significant (structural) and measured about 36 degrees. MRI Scan of the whole spine was done and it showed a large cystic cavity in the spinal cord (syrinx) with herniation of the brain at the cranio spinal Junction. This is called as the Arnold Chiari Malformation. She also had hydrocephalus. Scoliosis associated with Arnold Chiari malformation is subclassified as "syndromic scoliosis". 13 year old female child with scolosis. She presented with worsening deformity and rib hump.
Scoliosis with Arnold Chiari malformation on MRI. Patient has a large syrinx extending from upper cervical spine to lower thoracic spine.
Normally, the cerebellum sits at the back of the skull, just above the spine. When a child has a Chiari malformation, the space for the cerebellum is sometimes too small or unusually shaped. This can squeeze part of the cerebellum and even part of the brain down through a funnel-like hole below the skull. This hole is called the foramen magnum. A Chiari malformation can put pressure on the cerebellum, brain stem, and spinal cord and can keep those body parts from working properly. It also can block the movement of cerebrospinal fluid (CSF), the liquid that surrounds the brain and spinal cord and protects them from injury. When cerebrospinal fluid doesn't flow properly, it can cause hydrocephalus i.e a buildup of cerebrospinal fluid in the brain and spinal cord). This buildup can block communication of the brain's messages to the body and cause headaches, pain, numbness, and weakness.
The problem list can be summarized as:
1. Worsening Spine deformity with main structural cure of 85degrees.
2. Arnold chiari malformation.
3. Large Syrinx from upper cervical to lower thoracic spine.
4. Hydrocephalus
The Surgery: The Surgery is these patients are associated with significant risk of getting paralysis. The Surgery was planned in stages by Dr Abhijit Pawar. At stage one the decompression of the cranio vertebral junction (foramen magnum) was planned to remove the outflow obstruction to the cerebrospinal fluid. Surgery was done under neuromonitoring successfully. The child was observed for serial follow up for six month and the MRI was repeated at the end of 7 month. The follow up MRI showed the syrinx had significantly decreased in size.
X-ray picture showing good correction of spinal deformity and restoration of alignment.
The final scoliosis correction was planned. The major thoracic deformity and other 2 curves were corrected under precise neuromitoring. MEP and SSEP were monitored by the neurophysician continuously to ensure the patient does not get paralysis. All pedicle screws were placed on the concave side of the deformity and alternate on the convex side. Computer guided navigation techniques were used for placement of pedicular screws which ensure safe placement and minimal exposure to radiation. Precautions were taken to minimize the blood loss. The surgery was complete in about 5 hrs and the patient was shifted to recovery room in normal neurological condition. The pain was controlled post operatively by the expert pain management team at Kokilaben. The next day in the morning the child was made to sit and stand bed side. Active physiotherapy and walking was started on day 2. On 4 th post operative day the child was discharged. The child started going to school 1 month post surgery. She is not active and gets involved in sports 4 month post surgery.
Background: The female had severe back pain and bilateral leg pain. She was 150 kg in weight and mostly confined to the bed because of pain. She had multiple medical problems like Obstructive Sleep Apnoea. She could not lie down comfortably due to pain. The patient could hardly walk due to pain and weakness. Crippling back pain and leg pain throughout the day and more in the night made her life miserable. Patient used to spend several nights without sleep.
Diagnosis: X-ray showed Spondylolisthesis at L5-S1 i.e. slippage of vertebrae over each other. MRI showed Lumbar Spinal Stenosis i.e. severe narrowing of spinal canal. It was clear that she needed surgery to treat the problem. Doing open spinal surgery would be associated with huge risk due to medical problems. It would also increase the risk of infection and blood loss.
Due to disability from crippling back pain and leg pain, minimally-invasive fusion was planned. Doing minimally-access surgery in such morbidly obese patient was a difficult task. Special long instruments for the surgery were made ready and the surgery was planned.
Minimally-Access Surgery: Guide wires were placed under fluoroscopy control. Position of guide wires was confirmed on X-ray. With tubular retractors decompression was done and interbody fusion was done. Minimally-invasive PLIF was done successfully by Dr Abhijit Pawar. The procedure was complete in 2.5 hrs with almost no blood loss.
Recovery: On post operative day 2, patient was relieved of her back pain and leg pain. She started walking without support. On post operative day 5, the patient was discharged. Now she walks for longer duration and also sleeps well. Family is glad that she underwent this advanced procedure and her quality of life has dramatically improved.
52 years old Male Mr Pravin Pawar had a large tumour in his sixth thoracic vertebrae. He had weakness in legs as a result of the tumour compressing on the spinal cord.
Investigations were done at Kokilaben hospital showed large haemangioma in the 6th thoracic vertebrae. Haemangioma is a vascular tumour with rich blood supply. Removing a haemangioma in vertebral body has a risk of torrential bleeding and death. There was also a risk of spinal cord injury and complete paralysis.


Fig.1 & 2 Hemangioma at D6 Vertebral body causing spinal compression
Praveen came with some hope at Kokilaben after several opinions.
Investigations were done and surgery was planned in stages.
Stage 1: The interventional radiologist embolized the tumor on Day 1. Complete embolization of all vessels was done.
Stage 2: The decompression and excision of sixth thoracic vertebrae was planned. The vertebra was approached from the posterior approach. Verterbrectomy of thoracic 6th vertebrae was done. Neuromonitoring was used in all stages to ensure safety of surgery. Cage was placed anteriorly and posterior spinal instrumentation was done. As a result of embolization there was minimal bleeding during surgery. Histopathology however showed this tumor as plasmacytoma. Radiotherapy was done. At the end of month patient had a wonderful recovery was back to walking again. With multidisciplinary approach the patient is back to walking.

Fig.3 Post operative radiograph showing complete excision of tumour and posterior spinal stabilization
16 years old male Akash sustained injury to his head while playing Kabbadi. The injury was neglected. He had a dislocation of this cranium (skull) over his cervical spine. By the time he arrived in Kokilaben he was not able to walk due to paralysis. Young paralyzed child was investigated at Kokilaben. MRI and CT scan was done and it showed an old complete dislocation of first cervical vertebrae over the 2nd cervical vertebrae with severe spinal cord compression. The second cervical vertebrae had migrated in the cranium as a result of dislocation.

Fig.1.Dislocation of C1 over C2 with spinal cord compression
Cranio- Vertebral junction is a very precarious area with lot of vital centers of brain including the respiratory center. The dislocation was old and was a challenging task to reduce the dislocation. Parents of Akash had taken several opinion all over Maharashtra and came to Kokilaben Hospital with some hope that Akash would walk again.

Fig.2. Migration of C2 in the Cranium
The nature of complexity was discussed in details with parents. There was a risk of complete paralysis or even respiratory compromise post surgery. The surgery was planned in 2 steps
Stage 1: Transoral release of the dislocation was done along with the plastic surgery team.
Stage 2: Patient was tilted at the same day and the posterior aspect was exposed from the skull to upper cervical spine. Screw were placed in the Cranium and first and 2nd Cervical Vertebrae . Decompression of the cranio vertebral junction was done. All nerves were continuously monitored during the procedure to ensure safe spine surgery. The dislocation was reduced with rods placed between the skull and cervical vertebrae. Special care was taken not to injure the vertebral artery and other vital neural structures. Surgery was uneventful and Aakash was out of anesthesia.

Fig.3. Reduction of dislocation and alignment restored.
Patient recovered well and started walking normally.
At the end of one month with physiotherapy Aakash had completely recovered. He was back to school and sports. For the parents to see paralyzed Aakash walk was a dream come true. The complex spine surgery was successful with Aakash a completely normal child now.
This appointment request is for regular consultation with the Doctor at Kokilaben Hospital, Four Bungalows. For online consultation, please CLICK HERE
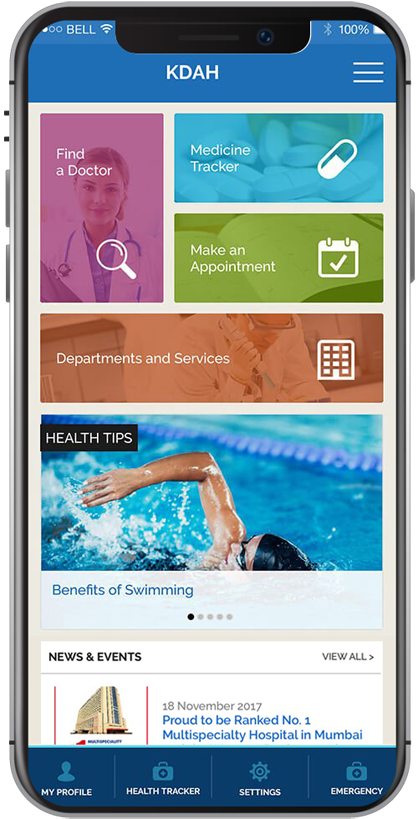
Stay updated to all the latest news and offers at KDAH
