Deep Brain Stimulation (DBS) surgery/programming is a therapy that can improve quality of life when medication management cannot be further optimized.
DBS surgery/programming is not a cure for Parkinson’s disease, Essential tremor, or Dystonia. DBS can provide symptomatic benefit, similar to maximal benefit achieved with medications, but with reduced motor fluctuations. In some cases, DBS may provide benefit beyond that achieved with medications alone.
DBS therapy can benefit motor symptoms of Parkinson’s disease including tremor (shakiness), rigidity (stiffness), and bradykinesia (slowness).
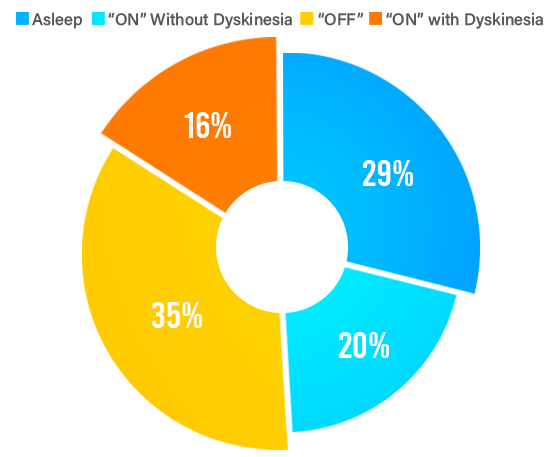
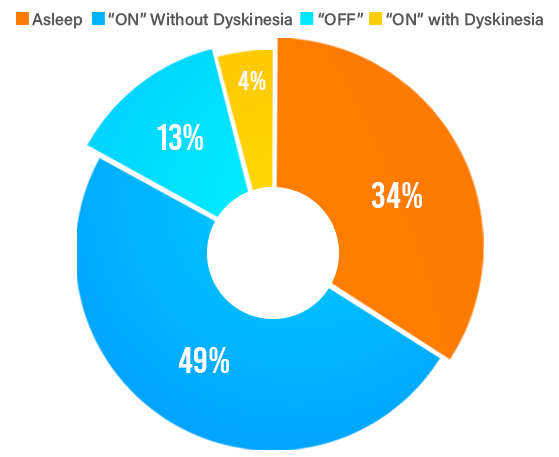
DBS can provide best “ON”time that you experience with your medications for PD, and a smoother therapy overtime that reduces motor fluctuations between “OFF”and “ON”periods throughout the day.
DBS therapy can also benefit patients with medicine induced dyskinesia (involuntary movement), as well as medication-refractory tremor, rigidity, and slowness of movements. Many patients who are not able to tolerate higher doses of medication due to side-effects may benefit from DBS. Most people will continue taking medications for PD after DBS surgery; however, DBS programming the amount of medication is often reduced.
Non-motor symptoms of Parkinson’s disease are typically not improved with DBS therapy. Symptoms such as constipation, urinary symptoms, and mood, memory, or sleep difficulties are not predicted to improve.
DBS may not be helpful in patients who do not experience any benefit from their medications; however, this patient should be evaluated by a Movement Disorder Neurologist to determine if they receive the correct medications at sufficient doses. Some patients who may suffer or benefit from higher doses of medications, but are unable to tolerate higher doses due to side-effects (such as sedation, lightheadedness, etc.) may benefit from DBS.
DBS therapy can significantly improve symptoms of Essential tremor, usually superior to the best medical therapy. Patients with Essential tremor may have tremors in the hands, head, and/or voice. Typically, DBS improves hand tremors more than head or voice tremors.
DBS can be effective therapy and dystonia, especially in patients with generalized and primary forms of dystonia. DBS may help patients with other forms of dystonia if medical therapy fails, but the rate of respondents maybe lower.
The DBS initial programming period could take 6 months to one year before symptoms of dystonia improve.
As part of the DBS evaluation to establish candidacy, you are asked to complete evaluations by a Neurologist, Neurosurgeon, Neuropsychologist, Speech specialist and a Physical therapist. These evaluations help us to determine the best management plan for your care.
The movement disorders neurologist who specializes in DBS at our clinic is Dr. Mohit Bhatt. A movement disorder neurologist or their physician assistant may videotape your examination during this evaluation.
For patients with diagnosis of Parkinson’s disease you will undergo an “ON-OFF evaluation”. You will come to the appointment “OFF”medications. You are asked to hold the medications that you take for Parkinson’s disease 12 hours prior to evaluation. You are to bring your medications for Parkinson’s Disease to this visit.
You will first be examined using a clinical little scale during an “OFF”medication state. You will then be asked to take your medications. The examination will be repeated during your “ON”medical medication state. The total evaluation often lasts for 1- 2 hours. Please keep in mind that if you have difficulty walking during your “OFF”medication state, then you should bring a wheelchair or walker to the appointment.
For patients with Essential tremor or Dystonia an “ON”/ “OFF”medical evaluation may not be completed in one sitting. However, these examinations may be videotaped.
Once these evaluations are completed, we will discuss your case after Multidisciplinary Movement Disorders Team Meeting. This information will allow the team to determine the best treatment plan for you. After the meeting, we will discuss the plan with you either by phone or in a follow-up clinic visit.
The DBS surgical procedure performed by our neurosurgeons are carried out in two stages.
The awake, MER guided procedure is best suited for patients, as they can communicate with the team during the procedure and possibly participate in the neurophysiology recording. This increases the efficacy and reduces the side-effects of electrical stimulation. It also helps doctors to locate the best position to implant and fix the final electrode.
Please discuss with your Neurologist and Neurosurgeon the details of the surgical procedure and the type of procedure best suited for you.
If the DBS team determines that you are a candidate for DBS surgery, and you wish to proceed with surgery, then the following will be arranged by the Neurosurgery team:
Continue your medication for Parkinson’s disease during this time. We stop the anti-Parkinson drugs the night before surgery. You will restart and continue these medications after surgery. Medications may be adjusted at the first initial programming visit after surgery.
You are required to complete basic preoperative testing before your upcoming surgery. The testing should be no later than seven days prior to your surgery date. We usually admit the patient on first day of the week and work up the patient. Patient undergoes the planning MRI scan, the neuro-psychological review, gait and speech assessment over the next three days. The history, blood works and other relevant tests are completed within these days. If you need medical clearance by a specialist, such as a cardiologist, the appointments are arranged during this period of time. Any specialized testing that needs to be done prior, for giving clearance for surgery is also conducted.
You need to discontinue your Parkinson’s medications the night before surgery. You may not eat or drink eight hours before your surgery (Wednesday night). Unless otherwise directed, on the morning of your surgery you may take any regularly scheduled medications with a small sip of water. The surgery usually takes place on Thursday morning wherein you will be shifted to the operation theatre.
Remember to discontinue any medication that increases bleeding risks for seven days prior to surgery (see attached list of medications to avoid before surgery). If you do take any blood thinning medication within a week of surgery, the surgery will be cancelled and rescheduled for a later date. If you experience any mild pain or headache within one week of surgery, the only approved over-the-counter pain medication to take is paracetamol or its generic equivalent acetaminophen.
After the surgery you will be monitored for 24 hours in the ICU. The Parkinson’s medication would be re-started. A CT scan of brain is performed the next morning after surgery. Subsequently you will be shifted to the wards with continued to be administration of IV antibiotics. The surgical site would be dressed on day 2 and day 4 from the day of surgery. Discharge from the hospital is usually scheduled a week later (on the next Tuesday) from the day of admission.
Potential risks of surgery include complications of bleeding or infection.
INFECTION PREVENTION:
Infection is a risk of any surgery, but an infection can be more serious in surgeries where a foreign device is placed in the body. We take every precaution to prevent this from happening, and now there is something you can do to help.
Bactoscrub/ Microshield (Chlorohexidine Gluconate 4% solution) Bactoscrub is a medicated soap that kills germs that normally live on your skin. Its use has been shown to reduce the risk of surgical infection.
MRSA is a “superbug” that is resistant to many antibiotics. Many people have this bacterium living on the skin, and it does not cause an infection. However, when the skin is cut, like in surgery, the bacteria can infect the wound. We want to identify the patients who are carriers of MRSA and treat them before surgery to decrease the risk of this particular infection. We can do this by simply taking a culture from your nose with a cotton swab. A negative MRSA culture report is desirable prior to the surgery. Additionally, Mupirocin ointment would be prescribed, to be applied inside both the nostrils twice daily for 3-4 days before surgery.
Some drugs potentially increase the risk of bleeding during surgery.
If you have any questions about medication to avoid prior to surgery, please contact the DBS team.
The first initial programming visit may take 1.5-2 hours. During the visit the clinician will turn the device therapy “ON”. Each electrode has four contacts. Each contact will be activated individually and the voltage slowly increased. As the voltage is increased you may experience benefit to symptoms or side-effects. The side-effects may be quickly reduced when the voltage is decreased. This process provides the clinician with information regarding the placement of electrode and the settings that will provide the best benefit for your symptoms. The goals of the DBS programming include improving symptoms while avoiding side-effects. Most side-effects of DBS programming are explained at the initial programming visit; however, in some instances Side effects can be delayed. Please call our clinical associate if you experience delayed side-effects.
During the initial programming visit you may experience side-effects of stimulation such as numbness, tingling, slurred speech, balance difficulty, facial pulling, or vision changes. The symptoms may be temporary, but you must let your DBS programmer know so that he or she may change the settings and reduce these symptoms.
Optimizing DBS programming may take up to 6 months. During this period, we are also adjusting the medications. Medications may be reduced once DBS programming is initiated.
Our expert team consists of:

Movement Disorders and Deep Brain Stimulation

Neurosciences/Neurosurgery, Minimal Access Surgery
Brain Tumour Surgery, Minimal Invasive Spine Surgery, Trigeminal Neuralgia Surgery, Stereotactic Radio surgery, Paediatric Neurosurgery

Function preserving tumor surgery with IONM, Deep Brain Stimulation Surgery, Peripheral Neuromodulation for pain and spasticity, Epilepsy Surgery

Anesthesiology, Neuroanesthesiology, Centre for Brain and Nervous system
